

#IRON STUDIES INTERPRETATION SKIN#
10,11Ĭ282Y homozygosity confers risk of the multi-organ consequences of iron overload, including liver fibrosis, liver cirrhosis, hepatocellular carcinoma, cardiac arrhythmias, cardiomyopathy, diabetes, arthropathy, hypogonadism and skin hyperpigmentation. 8,10 Even if H63D homozygotes develop elevated serum iron indices, they are unlikely to develop total body iron overload. C282Y homozygotes are at highest risk of developing total body iron overload whereas C282Y/H63D compound heterozygotes have much lower risk. This mutation has much higher penetrance than the H63D mutation. 9Īpproximately 1 in 200 people of Caucasian race are homozygous for the C282Y mutation. This mutation causes inappropriately increased intestinal iron absorption at a rate 2–3 times greater than normal.8 Similar to type 1 diabetes being a metabolic condition of glucose homeostasis due to insulin deficiency, HH is a metabolic condition of iron homeostasis due to hepcidin deficiency. Hereditary haemochromatosis is an autosomal recessive condition of progressive iron overload, usually due to homozygosity for the C282Y mutation in the HFE gene. Removal of 4 g or more of iron (16 weekly venesections) without developing iron deficiency anaemia indicates iron overload. In HH, total body iron stores can be calculated from the volume of blood removed during weekly venesections.

Whole blood contains 250 mg iron per 500 mL.
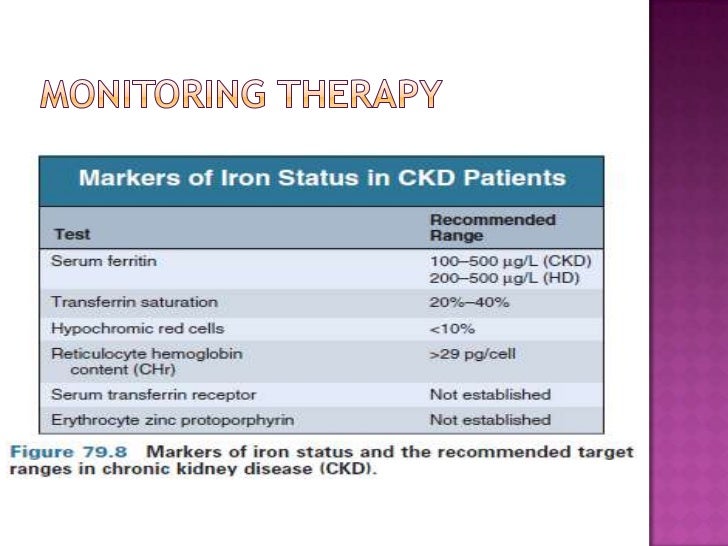
severe haemorrhage in haemophilia/surgery/traumaĪssessment of iron overload relies on surrogate markers, including serum tests (transferrin saturation, serum ferritin), noninvasive magnetic resonance imaging (MRI) scans for hepatic iron concentration (FerriScan®), liver biopsy and quantitative phlebotomy.red cell aplasia (congenital or acquired).Multiple transfusions to treat anaemia due to:.type 4: ferroportin mutation (FPN1 gene).type 3: transferrin receptor 2 mutation (TfR2 gene).type 2A: haemojuvelin mutation (HJV gene).Inappropriately increased intestinal iron absorption Causes of iron overload Mechanism of iron overload Table 2 outlines circumstances in which iron overload can develop. The human body lacks an iron excretion mechanism. Only 10% of daily dietary iron intake is absorbed. 7 Under the strict control of hepcidin, daily iron losses of 1–2 mg from sloughed mucosal, gastrointestinal and skin cells are accurately offset by daily absorption of 1–2 mg from dietary sources. Synthesised by the liver, the hormone hepcidin regulates total body iron levels by controlling intestinal iron absorption. Iron metabolismĪpproximately 75% of the body's 3–4 g total iron is found within haemoglobin in red blood cells, 10–20% is stored in the protein ferritin and the remainder is found in the iron transport protein transferrin, as well as in myoglobin, cytochromes and as unbound serum iron. Potential harms of frequent venesection therapy for a person without true iron overload include development of iron deficiency anaemia, reinforcement of a suboptimal management strategy for a biochemical abnormality, perpetuation of the myth that a genetic condition affecting family members exists, and the general venesection risks of venous scarring, phlebitis and vasovagal episodes. In the absence of contraindications, patients with elevated SF who do not meet eligibility criteria for therapeutic venesection may become volunteer whole-blood donors every 12 weeks. Options include private pathology providers, public hospitals, haematologists and some GPs. comorbid angina, hepatitis C, cerebrovascular disease) need to be referred elsewhere for therapeutic venesection. Patients meeting therapeutic venesection criteria with contraindications to volunteer blood donation (eg. Clinical iron overload supported by FerriScan ® MRI or liver biopsy.Evidence of hereditary haemochromatosis:.Eligibility criteria for Australian Red Cross Blood Service Therapeutic Venesection program While there is interest in iron reduction therapy for cancer risk reduction, 3 improvement of insulin sensitivity in metabolic syndrome 4 and management of fatty liver disease not responding to lifestyle changes, 5 the Australian Red Cross Blood Service Therapeutic Venesection program is currently restricted to patients meeting the criteria listed in Table 1, and who also meet the general eligibility criteria for volunteer blood donation.


 0 kommentar(er)
0 kommentar(er)
